 |
|
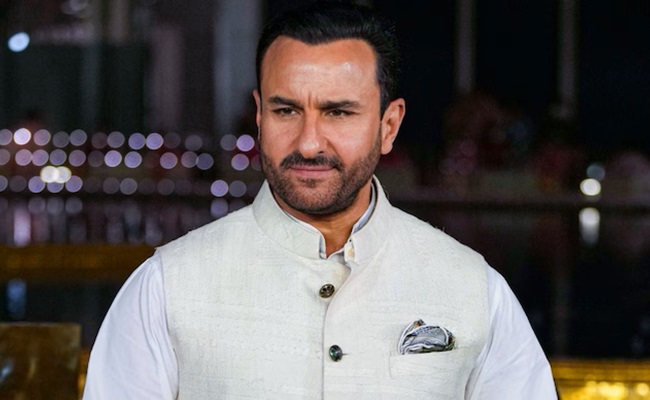
The recent swift processing of Saif Ali Khan's Rs 25 lakh cashless medical claim by Niva Bupa has ignited a significant debate regarding equity and transparency within India's insurance sector. The Association of Medical Consultants (AMC), a powerful voice representing over 14,000 medical professionals, has formally voiced its concerns to the Insurance Regulatory and Development Authority of India (IRDAI). Their letter highlights a perceived disparity in how claims are handled, suggesting that celebrities and high-profile individuals receive preferential treatment compared to ordinary citizens. This perceived bias, if proven, undermines the very foundation of insurance – the principle of equal protection and fair compensation regardless of social status.
The AMC's central argument revolves around the stark contrast between the rapid approval of Mr. Khan's claim and the experiences of numerous ordinary policyholders who often grapple with lengthy delays, insufficient coverage, and frustratingly low reimbursement rates. The organization points to a systemic issue where wealth and influence seem to disproportionately impact the claim approval process. This raises concerns about potential corruption and a lack of standardized procedures, questioning the impartiality of insurance companies in handling claims. The swift approval of Mr. Khan's claim, following a knife attack and subsequent surgery for multiple injuries, including a near-miss spinal cord injury, stands in stark contrast to the struggles faced by many others navigating the complexities of India's insurance system.
The call for transparency in determining claim approvals and cashless treatment limits is a crucial aspect of the AMC's complaint. The lack of clear, publicly available criteria for determining these limits leaves room for arbitrary decisions and potential bias. The AMC's request for an IRDAI investigation is a significant step towards addressing these concerns. An independent investigation can shed light on the processes employed by insurance companies, potentially revealing underlying discriminatory practices. Such an investigation could also lead to the development of clearer guidelines and regulations to prevent similar situations from arising in the future, ensuring fairness and equitable treatment for all policyholders, regardless of their social standing or public profile. The potential impact of this case extends far beyond a single celebrity's claim; it touches upon the fundamental principles of justice and fair access to essential healthcare services in India.
The incident with Saif Ali Khan’s insurance claim highlights a critical weakness in the Indian insurance system. The current lack of transparency and potential for bias undermines public trust and creates a two-tiered system where the wealthy and influential receive preferential treatment. This disparity is unacceptable and demands immediate attention from regulatory bodies. Moving forward, stricter regulations, robust oversight mechanisms, and a commitment to transparency are essential to ensure a fairer and more equitable system for all policyholders. The IRDAI’s response to the AMC's concerns will be crucial in determining the future direction of the Indian insurance industry and its commitment to providing equitable access to healthcare for all its citizens. Further investigation could reveal deeper systemic issues within insurance companies, requiring broad reforms to promote fairness and accountability.
The controversy surrounding Saif Ali Khan’s claim emphasizes the need for a complete overhaul of insurance claim processing. This includes the implementation of standardized procedures, transparent criteria, and robust oversight to minimize bias and ensure equitable treatment for all. The lack of clarity in the current system allows for arbitrary decisions, potentially leading to discrimination against those lacking the resources or influence to navigate the system effectively. Public pressure and strong regulatory action are needed to ensure that the principle of equal protection under the law extends to the realm of insurance claims, preventing future instances of perceived or actual preferential treatment based on social status or celebrity. The ultimate goal should be a system that guarantees fair and efficient processing of claims for all policyholders, regardless of their background or connections.
